Vascular Ehlers-Danlos Syndrome (VEDS) is a group of rare genetic disorders that affect the connective tissue in the body. The connective tissue is responsible for supporting and strengthening the body’s bones, organs, and other tissues. When this tissue is weakened due to a genetic mutation, it can cause a variety of symptoms and health complications. VEDS, also known as Vascular EDS (VEDS), is a particularly rare and serious form of EDS that can be life-threatening.
What is Vascular Ehlers-Danlos Syndrome?
Type 4 EDS or Vascular Ehlers-Danlos Syndrome (VEDS) is a rare genetic disorder that affects the body’s connective tissue. There are as many as 5,000 Americans with VEDS, and about 2,000 cases are known at this time. This form of Vascular Ehlers-Danlos Syndrome affects the blood vessels in the body. People with Vascular Ehlers-Danlos Syndrome have a genetic mutation that affects the production of type III collagen, which is a type of collagen that is found in the walls of blood vessels, intestines, and the uterus.
The weakening of blood vessels in people with VEDS can lead to a variety of health complications, including an increased risk of aneurysms, ruptured blood vessels, and organ rupture. In some cases, these complications can be life-threatening.
What are the Symptoms of Vascular Ehlers-Danlos Syndrome?
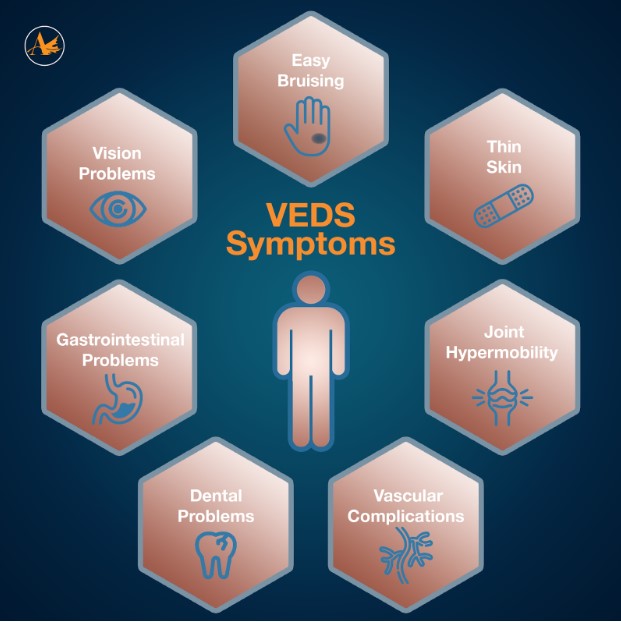
The symptoms of Vascular EDS can vary from person to person, and some people may have milder symptoms than others. However, there are several common symptoms that are associated with this condition. These symptoms include:
- Easy bruising – People with Vascular Ehlers-Danlos Syndrome may bruise easily, and the bruises may be larger and more noticeable than normal.
- Thin skin – The skin of people with Vascular Ehlers-Danlos Syndrome may be thin and transparent, and it may tear easily.
- Joint hypermobility – Bodies of those diagnosed with Vascular Ehlers-Danlos Syndrome may have joints that are more flexible than normal, which can increase the risk of dislocations.
- Vascular complications – Many with Vascular Ehlers-Danlos Syndrome may have an increased risk of aneurysms, ruptured blood vessels, and organ rupture.
- Dental problems – People with VEDS may have dental problems such as crowded teeth, weak enamel, or receding gums.
- Gastrointestinal problems – Individuals with Vascular Ehlers-Danlos Syndrome may experience gastrointestinal problems such as constipation and bloating.
- Vision problems – Those diagnosed with VEDS may have vision problems such as myopia and retinal detachment.
Other Vascular Ehlers-Danlos Syndrome symptoms may include:
- Large eyes that protrude
- Eye swelling and abnormal vision
- Thin nose
- Small jaw
- Hands that look older than they are
- Early onset varicose veins
- Chronic joint dislocations
- Club foot
It is important to note that not all individuals with Vascular Ehlers-Danlos Syndrome will experience all of these symptoms, and some may only experience a few. Additionally, some of these symptoms can be seen in other types of Ehlers-Danlos Syndrome or other connective tissue disorders, which can make diagnosis challenging.
Internal organ ruptures are a common complication in Vascular Ehlers-Danlos Syndrome. These ruptures can occur in the spleen, colon, uterus, and other organs. Internal bleeding caused by these ruptures can be fatal if not treated quickly. Spontaneous arterial rupture is another common complication, with up to 80% of individuals with VEDS experiencing at least one arterial rupture in their lifetime (1). Arterial rupture can occur anywhere in the body, but it is most commonly found in the carotid artery, subclavian artery, or iliac artery (2).
Vascular Ehlers-Danlos Syndrome can also affect the skin, causing it to be thin, translucent, and easily bruised. The skin may also be hyperextensible, meaning it can be stretched beyond what is considered normal. The presence of visible veins under the skin, particularly on the chest and abdomen, is another common symptom (3). Additionally, joint hypermobility is often present in individuals with Vascular Ehlers-Danlos Syndrome. This can lead to joint pain, dislocations, and arthritis.
No primary eye abnormalities have been described in VEDS, however there can be problems with the eyes caused by aneurysms of brain vessels or by hemorrhage in or behind the eye. In those cases, proptosis (protruding of the eye), motility disturbances of the eye or redness and
oedema of the conjunctiva may be seen (4).
What Causes Vascular Ehlers-Danlos Syndrome?
Vascular Ehlers-Danlos Syndrome is caused by mutations in the COL3A1 gene, which encodes for type III collagen, a major component of blood vessels and organs. Type III collagen is particularly important in blood vessels, where it helps to provide strength and support to the walls of the vessels. Mutations in the COL3A1 gene can lead to the production of abnormal type III collagen or a reduced amount of the protein, resulting in weakened blood vessels and organs (5).
VEDS is an inherited disorder, which means that it is passed down from parents to their children. It is inherited in an autosomal dominant manner, meaning that a person only needs to inherit one copy of the mutated gene from a parent to develop the condition. Individuals with VEDS have a 50% chance of passing the condition on to each of their children. However, it is important to note that up to 50% of cases of VEDS occur due to a de novo mutation, meaning that the mutation occurred spontaneously and was not inherited from a parent (6).
Vascular Ehlers-Danlos Syndrome is a rare genetic disorder that affects the connective tissue in the body. It is caused by mutations in the COL3A1 gene, which provides instructions for making a protein called type III collagen. This protein is a major component of the connective tissue in blood vessels, skin, and other organs. Mutations in the COL3A1 gene can result in the production of abnormal type III collagen, which can weaken the walls of blood vessels and other tissues, leading to potentially life-threatening complications.
What is a Gene and How Does it Mutate?
Genes are segments of DNA that provide the instructions for making proteins, which are the building blocks of the body. Genes can mutate, or change, in a variety of ways, and these mutations can have a range of effects on an individual’s health and well-being.
Types of Gene Mutations:
- Point mutations: Point mutations are the most common type of gene mutation. They involve a change in a single nucleotide, which is the basic unit of DNA. There are three types of point mutations: silent, missense, and nonsense.
- Silent mutations: Silent mutations are mutations that do not affect the amino acid sequence of the protein that is being made. This is because the genetic code is redundant, and different codons can code for the same amino acid.
- Missense mutations: Missense mutations are mutations that result in a change in the amino acid sequence of the protein that is being made. This can alter the function of the protein and can have a range of effects on the individual’s health.
- Nonsense mutations: Nonsense mutations are mutations that result in the premature termination of the protein that is being made. This can lead to a non-functional protein or a truncated protein that is unable to perform its intended function.
- Insertions and deletions: Insertions and deletions are mutations that involve the addition or removal of nucleotides from the DNA sequence. This can cause a shift in the reading frame of the genetic code, which can result in a non-functional protein.
- Duplications and deletions: Duplications and deletions are mutations that involve the duplication or deletion of large segments of DNA. These mutations can result in the loss or gain of genetic material and can have a range of effects on the individual’s health.
- Chromosomal abnormalities: Chromosomal abnormalities are mutations that involve changes in the structure or number of chromosomes. These mutations can have a range of effects on the individual’s health, including developmental abnormalities, intellectual disability, and increased risk of cancer.
Causes of Gene Mutations:
- Spontaneous mutations: Spontaneous mutations are mutations that occur naturally as a result of errors in DNA replication or DNA repair mechanisms. These mutations can occur randomly and are more likely to occur in cells that divide rapidly, such as those in the skin or the digestive tract.
- Environmental factors: Environmental factors, such as exposure to radiation, chemicals, or viruses, can increase the likelihood of gene mutations. For example, exposure to ultraviolet radiation from the sun can cause mutations in the DNA of skin cells, which can lead to skin cancer.
- Inherited mutations: Some gene mutations are inherited from one or both parents. These mutations can be passed down through generations and can increase the risk of certain genetic disorders, such as cystic fibrosis or Huntington’s disease.
Implications of Gene Mutations:
The effects of gene mutations can vary widely depending on the type of mutation and the gene that is affected. Some mutations may have no effect on the individual’s health, while others can have serious implications.
- Genetic disorders: Gene mutations can result in genetic disorders, which are conditions that are caused by inherited gene mutations. These disorders can affect a range of bodily systems and can have serious health implications.
- Increased risk of cancer: Certain gene mutations can increase the risk of cancer by disrupting the normal functioning of genes that control cell growth and division.
- Drug metabolism: Gene mutations can affect how the body metabolizes drugs, which can impact the effectiveness and safety of certain medications.
- Evolutionary changes: Gene mutations can also drive evolutionary changes by creating new variations in the genetic code that can be passed down to future generations. These changes can be beneficial, harmful, or have no effect on the survival of the individual or population.
- Genetic testing and counseling: Gene mutations can also have implications for genetic testing and counseling. Individuals who have a family history of genetic disorders or who are at increased risk of certain genetic disorders may choose to undergo genetic testing to identify any mutations that may be present. This information can be used to inform medical decisions and to provide genetic counseling to family members.
Gene mutations are changes in the DNA sequence that can have a range of effects on an individual’s health and well-being. These mutations can occur spontaneously, as a result of environmental factors, or as inherited mutations. Understanding the different types of gene mutations and their implications is important for identifying and managing genetic disorders, reducing the risk of cancer, and informing medical decisions and genetic counseling.
How Does the COL3A1 Gene Mutate?
The COL3A1 gene is located on chromosome 2 and contains 52 exons, which are the regions of the gene that contain the instructions for making the protein. Mutations in any of these exons can affect the production of type III collagen, leading to Vascular Ehlers-Danlos Syndrome.
VEDS is inherited in an autosomal dominant pattern, where only one copy of the mutated gene is needed to develop the condition. If a parent has VEDS, there is a 50% chance that their child will inherit the mutated gene and develop the condition.
Genetic counseling is also an important aspect of managing Vascular Ehlers-Danlos Syndrome. This involves meeting with a genetic counselor who can provide information about the inheritance pattern of the condition and the risks of passing it on to future children. Genetic testing can also be performed to determine whether other family members are at risk of developing Vascular Ehlers-Danlos Syndrome.
Vascular Ehlers-Danlos Syndrome is a rare genetic disorder that is caused by mutations in the COL3A1 gene. This can result in the production of abnormal type III collagen, which can weaken the walls of blood vessels and other tissues, leading to potentially life-threatening complications. Diagnosing Vascular Ehlers-Danlos Syndrome can be challenging, and treatment is focused on managing symptoms and preventing complications. Genetic counseling is an important aspect of managing Vascular Ehlers-Danlos Syndrome, as it can help individuals and families understand the risks of passing the condition on to future generations.
Genetic Counseling for COL3A1 gene mutation and Vascular Ehlers-Danlos Syndrome Diagnosis
Genetic counseling can be a valuable resource for individuals with Vascular Ehlers-Danlos Syndrome and their family members. This type of counseling involves meeting with a healthcare professional who specializes in genetics and genetic testing. The counselor can help individuals understand the inheritance pattern of the condition, and provide information on the risk of passing the mutated gene on to future generations.
Genetic counseling can also help individuals with Vascular Ehlers-Danlos Syndrome and their family members make informed decisions about family planning. For example, some individuals may choose to undergo prenatal testing to determine if their child has inherited the mutated gene. Others may choose to adopt or use assisted reproductive technologies, such as in vitro fertilization with preimplantation genetic diagnosis, to reduce the risk of passing the condition on to their children.
In addition to providing guidance on family planning, genetic counseling can also offer emotional support and resources for coping with a diagnosis of Vascular Ehlers-Danlos Syndrome. This can include connecting individuals with support groups and other resources for individuals and families affected by the condition.
Genetic counseling, pre-pregnancy counseling and management during pregnancy by
specialist fetal maternal teams will also be an essential part of the care of pregnant women
with this disorder. Provision of appropriate counseling for family planning will also be
necessary as pregnancy is associated with death in about 5% of women (7).
How is Vascular Ehlers-Danlos Syndrome Diagnosed?
Diagnosing Vascular Ehlers-Danlos Syndrome can be challenging, as the symptoms of Vascular Ehlers-Danlos Syndrome can be similar to other conditions. A diagnosis of Vascular Ehlers-Danlos Syndrome is typically based on a combination of clinical evaluation, family history, and genetic testing.
During a clinical evaluation, a healthcare provider may look for signs and symptoms of VEDS, such as easy bruising, thin skin, joint hypermobility, and vascular complications. They may also take a detailed family history to look for patterns of inheritance.
Genetic testing can be used to confirm a diagnosis of VEDS. This may involve analyzing a blood or saliva sample for the genetic mutation that causes the condition. Genetic testing can also be used to screen family members of a person with VEDS for the mutation.
It is important to note that genetic testing for Vascular Ehlers-Danlos Syndrome is not always accurate, and false-negative and false-positive results can occur. Therefore, a diagnosis of VEDS should be made by a healthcare provider who is experienced in diagnosing and managing this condition.
If you suspect you or someone you know may have VEDS, it is important to speak with a healthcare provider who is experienced in diagnosing and managing this condition.
Learn how we can help by joining our clinical treatment study for VEDS.
How Do You Treat and Manage Ehlers-Danlos Syndrome?
There is currently no cure for Vascular Ehlers-Danlos Syndrome, and treatment is focused on managing the symptoms and complications of the condition. This may involve a combination of medical and surgical interventions, depending on the individual’s specific needs.
Some of the treatments and management strategies for Vascular Ehlers-Danlos Syndrome include:
- Blood pressure management – Keeping blood pressure under control is important in people with VEDS, as high blood pressure can increase the risk of vascular complications.
- Surgery – In some cases, surgery may be necessary to repair or reinforce weakened blood vessels or other tissues.
- Medications – Medications may be prescribed to help manage symptoms such as pain and inflammation.
- Lifestyle modifications – Lifestyle modifications, such as avoiding activities that could cause injury and eating a healthy diet, can help reduce the risk of complications in people with VEDS.
- Regular monitoring – Regular monitoring, including imaging tests and check-ups with healthcare providers, is important in people with Vascular Ehlers-Danlos Syndrome to detect and manage complications early.
There is currently no cure for Vascular Ehlers-Danlos Syndrome, so treatment is focused on managing symptoms and preventing complications. This may include regular monitoring for arterial aneurysms or dissections, and surgical intervention if necessary. Blood pressure control is also important, as high blood pressure can increase the risk of arterial rupture.
Individuals with Vascular Ehlers-Danlos Syndrome should also take steps to protect their skin and avoid activities that could lead to injury, such as contact sports. They may also benefit from working with a physical therapist or occupational therapist to develop exercises and techniques to help strengthen joints and prevent injury.
Vascular Ehlers-Danlos Syndrome is a rare genetic disorder that affects the connective tissue in the body. It is caused by mutations in the COL3A1 gene, which is responsible for producing a protein called type III collagen. This protein is essential for the strength and elasticity of blood vessels, organs, and other tissues in the body. Vascular Ehlers-Danlos Syndrome is a subtype of the disorder that specifically affects the blood vessels, causing them to be fragile and prone to rupture. This can lead to a variety of symptoms and health complications, including an increased risk of aneurysms, ruptured blood vessels, and organ rupture. Diagnosing VEDS can be challenging, but a combination of clinical evaluation, family history, and genetic testing can help confirm a diagnosis. Treatment and management of Vascular Ehlers-Danlos Syndrome is focused on managing symptoms and complications, and regular monitoring is important to detect and manage complications early. Genetic counseling can also be a valuable resource for individuals and families affected by the condition, providing guidance on family planning and emotional support.
Be part of advancing the treatment of VEDS with this exciting new study. The DiSCOVER Trial is a decentralized study evaluating Celiprolol on VEDS-related events in individuals with confirmed diagnosis of Vascular Ehlers-Danlos Syndrome who meet specific criteria. If you pre-qualify, a Science 37 Patient Experience Coordinator will contact you within 24 hours via a phone call to discuss the study in more detail.
To be eligible for the Discover Celiprolol trial, individuals must have a confirmed diagnosis of VEDS based on genetic testing and meet specific clinical criteria, be at least 15 years old, and not currently pregnant.
Individuals with Vascular Ehlers-Danlos Syndrome who meet certain criteria have found celiprolol to be effective in reducing the risk of arterial and organ rupture. As a beta-blocker medication, celiprolol works by alleviating the stress on blood vessels and other organs, which reduces the risk of rupture.
Acer Therapeutics is actively seeking potential participants with a confirmed diagnosis of Vascular Ehlers-Danlos Syndrome caused by a COL3A1 mutation who are interested in participating in this investigational trial.
If eligible, participation is remote so you can continue living as you normally do. A registered nurse visits your home, and periodically study visits will be conducted online. All instructions will be provided, and the investigational drug will be shipped directly to you.
Celiprolol is an investigational drug and therefore its safety and efficacy have not been established. There is no guarantee that celiprolol will receive health authority approval or become commercially available for Vascular Ehlers-Danlos Syndrome.
Learn more and find out if you are eligible for the VEDS clinical trial.
Have more questions? Check out our FAQ for some answers.
REFERENCES:
- Pepin, M. G., & Byers, P. H. (2014). Ehlers-Danlos Syndrome Type IV. GeneReviews®.
- Demerath, E. W., Guo, X., & Rhodes, K. L. (1997). Rupture of the subclavian artery in Ehlers-Danlos syndrome type IV. Journal of vascular surgery, 26(6), 1066-1071.
- Tinkle, B., Castori, M., Berglund, B., Cohen, H., Grahame, R., Kazkaz, H., … & Malfait, F. (2017). Hypermobile Ehlers–Danlos syndrome (a.k.a. Ehlers–Danlos syndrome Type III and Ehlers–Danlos syndrome hypermobility type): clinical description and natural history. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175(1), 48-69.
- Wenstrup, R. J., Meyer, R. A., & Lyle, J. S. (2002). Ehlers-Danlos syndrome type IV: a multi-disciplinary approach to successful management. Clinical genetics, 62(5), 229.
- Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., … & Tinkle, B. (2017). The 2017 international classification of the Ehlers–Danlos syndromes. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175(1), 8-26.
- Germain, D. P. (2004). Ehlers–Danlos syndrome type IV. Orphanet Journal, 6(1), 15.
- Ong, K. T., Perdu, J., de Backer, J., & Bozec, E. (2018). Diagnosis and management of vascular Ehlers-Danlos syndrome: a consensus statement for inherited rare diseases from the European Reference Network on Rare Multisystemic Vascular Diseases (VASCERN). Orphanet Journal of Rare Diseases, 13(1), 1-17.
ADDITIONAL REFERENCES:
Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., … & Tinkle, B. (2017). The 2017 international classification of the Ehlers–Danlos syndromes. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175(1), 8-26.
Beighton, P., De Paepe, A., Steinmann, B., Tsipouras, P., & Wenstrup, R. J. (1998). Ehlers-Danlos syndromes: revised nosology, Villefranche, 1997. American Journal of Medical Genetics, 77(1), 31-37.
Frank, M., Albuisson, J., Ranque, B., Golmard, L., Mazzella, J. M., Bal-Theoleyre, L., … & Adès, L. C. (2015). The type of variants at the COL3A1 gene associates with the phenotype and severity of vascular Ehlers-Danlos syndrome. European Journal of Human Genetics, 23(12), 1657-1664.
Mayo Clinic. (n.d.). Mayo Clinic. Retrieved April 6, 2023, from https://www.mayoclinic.org/
National Library of Medicine. (n.d.). MedlinePlus. Retrieved April 6, 2023, from https://medlineplus.gov/