Vascular Ehlers-Danlos Syndrome (VEDS) is a rare genetic connective tissue disorder that affects the body’s blood vessels and organs, leading to a high risk of life-threatening complications. It is caused by mutations in the COL3A1 gene and is transmitted as an autosomal dominant trait (1). COL3A1 provides instructions for making type III collagen, a protein that gives structure and strength to blood vessels, skin, and other tissues.
VEDS is one of the most severe forms of Ehlers-Danlos Syndrome (EDS), a group of genetic disorders that affect the body’s connective tissues. It is estimated to affect 1 in 50,000 to 1 in 200,000 people worldwide, with no known cure (2). However, there are several treatment options available to manage the symptoms and reduce the risk of complications.
Research on VEDS
Research is ongoing to better understand the underlying causes of VEDS and to develop new treatments and management programs. Clinical trials are currently underway to test the safety and efficacy of new treatments for VEDS, including gene therapies and medications that target specific symptoms of the disorder. It’s important for individuals with VEDS to stay up to date on the latest research and to discuss any new treatment options with their healthcare provider.
Medical Management for TYPE 4 VEDS
The first line of treatment for VEDS is medical management, which includes regular monitoring and screening for complications, such as arterial dissection, aneurysms, and organ rupture. Early detection and treatment of these complications are essential to prevent life-threatening consequences.
Patients with VEDS should have regular follow-up appointments with a team of healthcare providers, including a geneticist, a cardiologist, a vascular surgeon, and a gastroenterologist, to monitor their condition and provide appropriate care. Imaging tests, such as echocardiography, magnetic resonance imaging (MRI), and computed tomography (CT) scans, are used to screen for complications and guide treatment decisions.
Experimental Therapies Studying VEDS
Currently, there are no specific treatments or cures for VEDS. However, several experimental therapies are being investigated to address the underlying genetic defect and improve the outcomes of patients with VEDS. These include:
- Beta Blockers: This approach measures the value of long-term beta blocker treatment (celiprolol) to prevent vascular complications in EDS type IV within the DiSCOVER Celiprolol study. Find more information here.
- Gene therapy: This approach aims to deliver a functional copy of the COL3A1 gene to the patient’s cells, using viral vectors or other gene delivery systems, to restore the production of normal type III collagen and improve the strength and stability of the blood vessels and tissues. Several preclinical studies have shown promising results in animal models of VEDS, but more research is needed to optimize the safety and efficacy of gene therapy in humans.
- Collagen replacement therapy: This approach involves the administration of exogenous collagen to the patient’s body, using synthetic or natural sources, to supplement the deficient type III collagen and enhance the structural integrity of the blood vessels and tissues. Some studies have suggested that collagen replacement therapy may improve the healing of skin wounds and reduce the incidence of arterial rupture in VEDS patients, but further clinical trials are needed to confirm its safety and efficacy.
- Pharmacological chaperone therapy: This approach aims to enhance the folding and stabilization of mutant type III collagen molecules, using small molecules or other compounds, to promote their secretion and function in the extracellular matrix. Several in vitro and in vivo studies have shown that pharmacological chaperones can improve the secretion and assembly of mutant type III collagen in VEDS fibroblasts and animal models, but their clinical applicability and long-term effects are still under investigation.
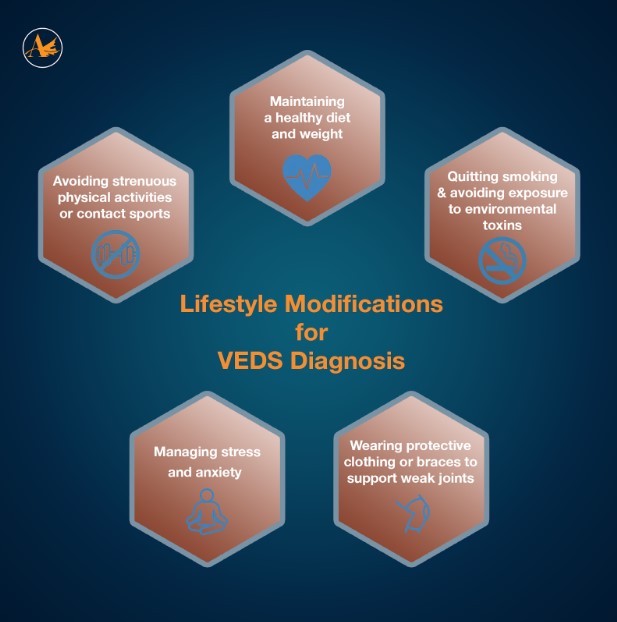
Lifestyle Modifications for VEDS Diagnosis
Patients with VEDS may benefit from lifestyle modifications to reduce the risk of complications and improve their quality of life. These include:
- Avoiding strenuous physical activities or contact sports that may increase the risk of trauma or injury to the blood vessels and tissues.
- Maintaining a healthy diet and weight to reduce the risk of hypertension, diabetes, and other metabolic disorders that can exacerbate VEDS symptoms.
- Quitting smoking and avoiding exposure to environmental toxins, such as air pollution or chemicals, that can damage the blood vessels and tissues and increase the risk of complications in VEDS.
- Managing stress and anxiety through relaxation techniques, such as deep breathing, meditation, or yoga, which can help reduce blood pressure and improve mental health.
- Wearing protective clothing or braces to support weak joints and prevent injuries, such as joint dislocation or fracture, that can aggravate VEDS symptoms.
Pain Management for VEDS
Many patients with Type 4 VEDS experience chronic pain, which can be difficult to manage. Treatment options for pain management may include nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, or other pain relievers, such as acetaminophen. However, because patients with EDS may be more sensitive to the side effects of these medications, it is important to work closely with a healthcare provider to determine the appropriate dosage and duration of treatment.
Medications to Manage VEDS Symptoms
Several medications may be used to manage the symptoms and reduce the risk of complications in patients with VEDS. These include:
- Beta-blockers: These drugs can help reduce blood pressure and heart rate, which can lower the risk of arterial rupture and dissection. They are often used in combination with other medications, such as ACE inhibitors or calcium channel blockers, to control blood pressure (3).
- Anticoagulants: These drugs can prevent blood clots from forming and reduce the risk of arterial thrombosis, which can lead to organ damage or failure. However, the use of anticoagulants in VEDS is controversial, as they can also increase the risk of bleeding and hemorrhage.
- Pain relievers: Patients with VEDS may experience chronic pain due to joint hypermobility, muscle weakness, or nerve compression. Over-the-counter pain relievers, such as acetaminophen or ibuprofen, may be used to manage mild to moderate pain. However, stronger opioids or other narcotic painkillers are generally not recommended, as they can increase the risk of gastrointestinal bleeding, cardiovascular complications, and addiction.
Wound Care in VEDS
Because the skin in patients with VEDS is often more fragile and prone to tearing, wound care is an important consideration. Patients should take steps to protect their skin, such as using gentle skin care products and avoiding activities that could lead to skin tears. If a wound does occur, it should be cleaned and dressed appropriately to prevent infection.
Joint Support for VEDS
Joint support is another important treatment option for patients with Type 4 VEDS. This may include physical therapy to strengthen muscles and improve joint stability, or the use of braces or other supportive devices to reduce stress on the joints. In some cases, surgery may be necessary to repair or replace damaged joints.
Surgery for Patients with VEDS
In some cases, surgery may be necessary to repair or replace damaged organs or tissues in patients with VEDS. However, because patients with VEDS are at increased risk of complications during and after surgery, it is important to work closely with a healthcare provider to determine the appropriate surgical approach and to take steps to minimize the risk of complications. Surgery may, however, be required urgently to treat potentially fatal complications such as uncontrolled hemorrhage or a very large or rapidly-expanding aneurysm (4). Surgical interventions should be carefully considered and planned by a multidisciplinary team of healthcare providers with expertise in VEDS. The timing and type of surgery may depend on the location and severity of the vascular or organ involvement, as well as the patient’s overall health status and preferences.
Vascular Ehlers-Danlos Syndrome and Genetic Counseling
Because VEDS is a genetic disorder, genetic counseling may be a useful treatment option for patients and their families. Genetic counseling can help patients and their families understand the underlying causes of the disorder, assess their risk of passing the disorder on to future children, and make informed decisions about family planning. Pregnant women with vascular EDS should be considered at risk and receive special care (5). Maternal mortality stands at around 12% (6).
VEDS Support Groups
There are many support options available for individuals with VEDS and their families, including online communities, local support groups, and national organizations. These groups can provide a source of emotional support, information, and resources for individuals with VEDS.
VEDS is a rare genetic disorder that poses significant challenges for patients and healthcare providers. While there is no cure for VEDS, several treatment options are available to manage the symptoms, reduce the risk of complications, and improve the quality of life of patients with VEDS. These include medical management, medications, surgery, lifestyle modifications, and experimental therapies. A multidisciplinary approach, involving a team of experts in VEDS management, is essential to provide personalized and effective care for VEDS patients. Further research is needed to develop and validate new therapies that can address the underlying molecular defects in VEDS and provide more durable and long-lasting benefits for patients. Find out more at DiSCOVER Celiprolol.
Scientific sources:
- Germain DP, Herrera-Guzman Y. Vascular Ehlers-Danlos syndrome. Ann Genet. 2004;47:1–9.
- Pepin, M. G., Schwarze, U., Rice, K. M., Liu, M., Leistritz, D., Byers, P. H., & Steiner, R. D. (2014). Survival is affected by mutation type and molecular mechanism in vascular Ehlers–Danlos syndrome (EDS type IV). Genetics in Medicine, 16(12), 881-888.
- Boutouyrie P, Germain DP, Fiessinger JN, Laloux B, Perdu J, Laurent S. Increased carotid wall stress in vascular Ehlers-Danlos syndrome. Circulation. 2004;109:1530–1535. doi: 10.1161/01.CIR.0000121741.50315.C2.
- Oderich, G. S., Panneton, J. M., Bower, T. C., Lindor, N. M., & Cherry, K. J. (2005). The spectrum, management and clinical outcome of Ehlers-Danlos syndrome type IV: a 30-year experience. Journal of Vascular Surgery, 42(1), 98-106.
- Germain, D. P. (2017). Ehlers–Danlos syndrome type IV. Orphanet Journal of Rare Diseases, 12(1), 1-8.
- Pepin M, Schwarze U, Superti-Furga A, Byers PH. Clinical and genetic features of Ehlers-Danlos syndrome type IV, the vascular type. N Engl J Med. 2000;342:673–680.
ADDITIONAL REFERENCES:
Bowen, J. M., Sobey, G. J., Burrows, N. P., Colombi, M., Lavallee, M. E., Malfait, F., … & De Paepe, A. (2021). Ehlers-Danlos syndrome, classical type. Nature Reviews Disease Primers, 7(1), 1-20.
Pepin, M. G., Murray, M. L., Byers, P. H., & Ehlers-Danlos Syndrome Type IV Collaborative Group. (2000). Therapeutic approach to patients with vascular complications of Ehlers-Danlos syndrome type IV. Genetic counseling, 11(3), 221-235.
Byers, P. H., Belmont, J., Black, J., De Backer, J., Frank, M., Jeunemaitre, X., … & Pepin, M. (2017). Diagnosis, natural history, and management in vascular Ehlers-Danlos syndrome. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175(1), 40-47.
Frank, M., Albuisson, J., Ranque, B., Golmard, L., Mazzella, J. M., Bal-Theoleyre, L., … & Boileau, C. (2015). The type of variants at the COL3A1 gene associates with the phenotype and severity of vascular Ehlers-Danlos syndrome. European Journal of Human Genetics, 23(12), 1657-1664.
Montalcini, T., Romeo, S., Ferro, Y., Migliaccio, V., Gazzaruso, C., & Pujia, A. (2018). Arterial stiffness, endothelial and cognitive function in subjects with vascular Ehlers-Danlos syndrome: a case control study. BMC Cardiovascular Disorders, 18(1), 1-8.
Fernández-Alonso, L., Pérez-San Gregorio, M. A., Velasco, E. A., Barrios, L. G., & Hernández-Martínez, A. (2021). Clinical management of patients with vascular Ehlers-Danlos syndrome: a review. Orphanet Journal of Rare Diseases, 16(1), 1-14.
Kolev, M., Todorova, A., & Kayserili, H. (2019). Successful management of arterial dissection in vascular Ehlers–Danlos syndrome with a staged endovascular approach: a case report. Vascular, 27(3), 318-322.
Lurie S, Manor M, Hagay ZJ. The threat of type IV Ehlers-Danlos syndrome on maternal well-being during pregnancy: early delivery may make the difference. J Obstet Gynaecol. 1998;18:245–248.
Malfait, F., Francomano, C., Byers, P., Belmont, J., Berglund, B., Black, J., … & Tinkle, B. (2017). The 2017 international classification of the Ehlers–Danlos syndromes. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175(1), 8-26.